Abstract
Background:
Patients with diffuse large B-cell lymphoma (DLBCL) are routinely treated in the outpatient setting. However, those who experience toxicity from a new diagnosis, relapsed disease, or outpatient chemotherapy may require inpatient admissions. Occasionally, patients with relapsed disease or a new diagnosis require inpatient chemotherapy. There is limited data on which patients are more likely to receive chemotherapy in the hospital, and which patients are more likely to suffer fatal complications during hospitalization. We examined patient and hospital characteristics associated with receiving inpatient chemotherapy and death during hospitalization for adults with DLBCL using a large US national database.
Methods:
We obtained admission data for patients with DLBCL from the 2012 and 2013 Agency for Healthcare Research and Quality's Healthcare Cost and Utilization Project National Inpatient Sample (HCUP-NIS). HCUP-NIS is a sampling of 20% of discharges from US hospitals, and provides weights that correspond to the total number of discharges represented by a single discharge in the dataset to provide national estimates. Utilizing existing variables in the HCUP-NIS database, including risk on the likelihood of dying, we performed univariate analysis of patient demographics associated with receipt of chemotherapy and death during hospitalization. We used multivariable logistic regression to identify predictors of death during hospitalization. The following factors were included: age, sex, income, insurance, number of chronic conditions, race, hospital type, region, length of stay (LOS), charges per day, and receipt of chemotherapy during the admission. All results apply the HCUP-NIS weights.
Results:
There were 10,860 admissions associated with DLBCL in 2012-2013. Median patient age was 70 years (IQR 59-78). Over half (55%) of admissions were of male patients. 3,170 (29%) of hospitalizations included administration of chemotherapy. Those who received chemotherapy in the hospital were younger (64 vs. 72 years, p<0.001), more often in urban teaching hospitals (p<0.001), had fewer chronic conditions (median 3.5 vs. 5.4, p<0.001), were more often male (31 vs. 27%, p=0.02), had private or Medicaid insurance (vs. Medicare, both p<0.001), and were less likely to have an "extreme likelihood of dying" per the HCUP-NIS database (4.9% vs. 11.4% p<0.001) than those who did not receive chemotherapy.
575 (5.3%) of hospitalizations resulted in death. Patients who died during hospitalization were older (median 74.6 vs. 69.4 years, p<0.001), had an extreme likelihood of dying (66% vs. 6.3% p<0.001), had more chronic conditions (5.9 vs. 4.7, p<0.001), experienced longer LOS (7 vs. 4 days, p<0.001) and more charges per day ($8,241 vs. $6,127, p<0.001) compared to those who did not die. Patients who had not received chemotherapy during admission were more likely to die compared to those who received chemotherapy (6.6 vs. 2.2%, p<0.001). There was no difference in hospital type (rural/urban-nonteaching, vs. urban teaching), sex, geographic region, race, and income quartile among those who did vs. did not die during hospitalization.
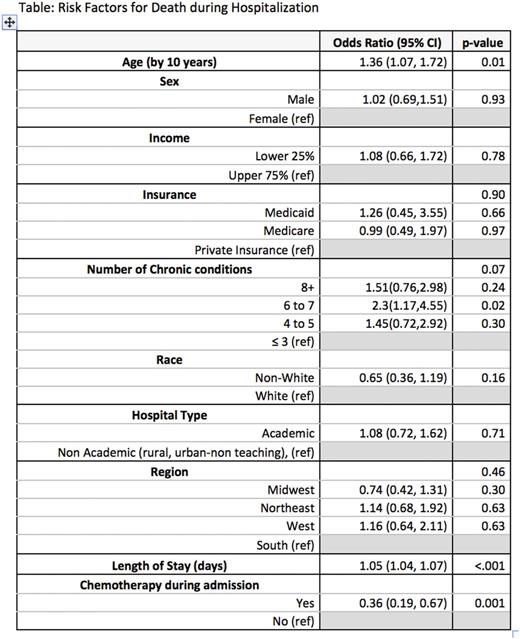
In multivariable regression, older age (OR 1.36 for 10-year increase, p=0.01) and longer LOS (OR 1.05, p<0.001were associated with higher odds of dying during hospitalization), while receiving chemotherapy (OR 0.36, p<0.001) was associated with lower odds of dying (Table).
Conclusions:
The majority of hospitalizations for patients with DLBCL did not include administration of chemotherapy. Those who received inpatient chemotherapy were generally younger and male, had less comorbidity, were admitted to urban teaching hospitals, and did not have Medicare insurance. A minority of hospitalizations resulted in death. Longer LOS and no receipt of chemotherapy were predictive of death during admission. Our data suggest that the majority of inpatient stays for DLBCL were unplanned admissions due to toxicity, and socio-demographics were not significant factors compared to clinical acuity in identifying who was at risk for death.
Kumar: Celgene: Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal